Ophthalmic Studies
A Novel Platform for Ocular Research
Pebble's LIVING-EYE System
The Pebble LIVING-EYE system replicates in-vivo physiology, circulating warm, nutrient rich, oxygenated blood through arteries and deoxygenated, nutrient depleted blood through veins. This restores metabolic function within the eye, providing an ideal platform for testing therapies and performing electroretinography.
Perfusion Protocols
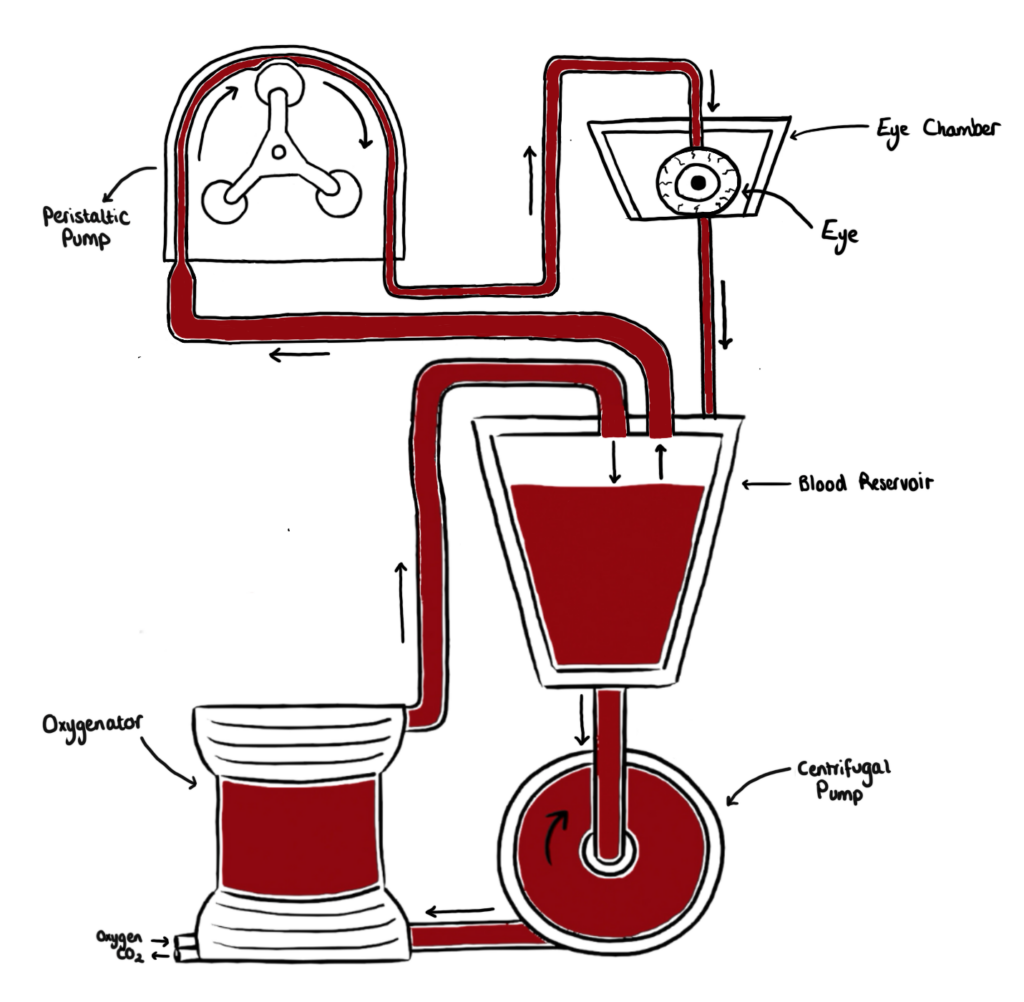
Eyes are perfused with autologous blood and maintained under physiological conditions.
Our LIVING-EYE System reproduces the living environment, providing an excellent platform for translatable testing. A warm, oxygenated blood-based perfusate is percolated through the ophthalmic vasculature, providing nutrients and enabling gas exchange to occur.
We only use clinical gold standard protocols for organ preservation (including approved cold-storage and machine perfusion approaches). All solutions, consumables and hardware are FDA/MHRA/EMA approved.
Our expert multidisciplinary team are keen to push the boundaries of perfusion, so if you have a project in mind, no matter the complexity, please get in touch.
Ophthalmic Study Evaluation
Study Design
- Photoreceptor Rescue Experiments: Testing the efficacy of neuroprotective agents in preventing photoreceptor cell death.
- Retinal Detachment Models: Simulating retinal detachment to study the effects of therapeutic interventions on retinal healing and scarring.
- Angiogenesis Inhibition Trials: Applying anti-angiogenic drugs to investigate their ability to prevent pathological neovascularization.
- Retinal Pigment Epithelium (RPE) Functionality: Examining the impact of treatments on RPE health, crucial for maintaining overall retinal architecture.
- Epithelial Integrity Experiments: Assessing the regenerative capacity of corneal epithelium after mechanical abrasion or chemical burns.
- Endothelial Permeability Tests: Evaluating the effects of drugs on corneal endothelial cell tight junctions and their ability to maintain corneal dehydration.
- Keratocyte Response Assays: Monitoring keratocyte behavior in response to corneal injuries or keratorefractive surgery procedures.
- Drug Penetration and Absorption Analysis: Measuring how therapeutic agents traverse the corneal layers, optimizing formulations for maximal efficacy.
- Trabecular Meshwork Flow Studies: Testing medications that aim to increase aqueous humor outflow through the trabecular meshwork.
- Neuroprotective Strategies for Optic Nerve Health: Evaluating compounds designed to protect retinal ganglion cells and the optic nerve from glaucomatous damage.
- Intraocular Pressure (IOP) Regulation: Assessing the ability of various compounds to modulate IOP, a critical factor in glaucoma management.
- Absorption Studies: Ex-vivo perfused eyes can be used to study the absorption of drugs across ocular tissues, including the cornea and conjunctiva. These studies can provide information on drug permeability and bioavailability.
- Distribution Studies: Researchers can investigate how drugs distribute within different ocular tissues and assess factors influencing drug distribution in the eye.
- Metabolism Studies: Ex-vivo models can be employed to study the metabolism of drugs within ocular tissues, providing insights into the biotransformation of drugs in the eye.
- Drug Release Profiles: Ex-vivo perfused eyes can be used to study the release kinetics of drugs from various formulations, including sustained-release implants or nanoparticles.
- Intraocular Injection Studies: Researchers can investigate the distribution and pharmacokinetics of drugs following intraocular injections (e.g., intravitreal injections) in the ex-vivo perfused eye model.
- Vascular Perfusion Studies: Ex-vivo perfused eyes allow for the study of vascular perfusion and blood flow in ocular tissues. This is crucial for understanding drug transport through the ocular vasculature.
- Drug Transport Across Barriers: Researchers can use the model to study the transport of drugs across ocular barriers, including the blood-retinal barrier, and evaluate factors affecting drug penetration.
- Absorption Kinetics: Measuring how quickly and effectively drugs are absorbed into various ocular tissues after different delivery methods.
- Distribution Mapping: Tracking the distribution of therapeutics throughout the eye to identify target tissues and potential off-target effects.
- Metabolism Profiling: Analyzing how drugs are metabolized within ocular tissues, identifying metabolites and understanding local metabolic pathways.
- Excretion Dynamics: Investigating the clearance of drugs and their metabolites from ocular tissues, determining half-lives and informing dosing schedules.
- Drug-Drug Interaction Studies: Ex-vivo perfused eyes can be used to assess potential drug-drug interactions when multiple medications are administered concurrently.
- Therapeutic Effectiveness: Ex-vivo perfused eyes can be used to assess the therapeutic efficacy of drugs in treating specific ocular conditions. For example, the model can be employed to study the effect of anti-glaucoma medications on intraocular pressure.
- Retinal Function Studies: Researchers can investigate the impact of drugs on retinal function by measuring parameters such as electroretinograms (ERGs) in the perfused eye model.
- Ocular Irritation and Tolerance: Ex-vivo perfused eyes can be exposed to drug formulations to evaluate potential irritation or adverse reactions. This is important for assessing the safety of ocular medications.
- Corneal and Retinal Toxicity: Researchers can use the model to study the potential toxic effects of drugs on ocular tissues, such as the cornea and retina.
- Cytotoxicity Assays: Assessing the potential toxicity of drugs to ocular cells, including apoptotic and necrotic responses.
- Irritation and Inflammation Responses: Evaluating the propensity of substances to induce irritation or inflammatory responses in ocular tissues.
- Ocular Tissue Integrity Tests: Monitoring the structural integrity of the eye under the influence of test substances to detect potential damage.
- Stem Cell Integration and Survival: Introducing stem cells to damaged ocular tissues and evaluating their integration and regenerative capacity.
- Gene Delivery Efficiency: Testing various vectors for gene therapy delivery, assessing transduction efficiency and expression levels in target cells.
- Regenerative Agent Screening: Identifying compounds that promote regenerative processes in ocular tissues, including neuroprotective agents for the retina.

Therapeutic Administration
- Eye Drops: This is the most common method for delivering drugs to the anterior segment of the eye (cornea, conjunctiva, and anterior chamber). However, penetration through the cornea can be limited due to its protective barriers, such as the corneal epithelium.
- Ointments & Gels: These are applied to the conjunctival sac and provide a longer contact time compared to eye drops. They are often used for sustained release of drugs.
- Subconjunctival Injection: This involves injecting drugs into the subconjunctival space, allowing for sustained release and avoiding the rapid tear clearance associated with topical applications.
- Sub-Tenon’s Injection: Similar to subconjunctival injection, this technique involves injecting drugs into the space between the sclera and Tenon’s capsule.
- Periocular Implants: Biodegradable implants or devices can be surgically placed in the periocular space for controlled and sustained drug release.
- Intravitreal Injection: This is a common method for delivering drugs directly into the vitreous humor. It is used for treating conditions affecting the posterior segment of the eye, such as retinal diseases.
- Intracameral Injection: This involves injecting drugs into the anterior chamber of the eye. It is used for treating conditions affecting the anterior segment, such as glaucoma.
- Intravitreal Implants: These are small, biodegradable implants placed in the vitreous cavity for sustained drug release over an extended period.
- Oral Medications: Systemic administration of drugs can sometimes reach therapeutic levels in the eye. However, systemic delivery may have limited effectiveness and potential side effects.
- Intravenous (IV) Administration: Intravenous infusion of drugs can also lead to systemic distribution, with some drugs reaching the eye.
- Transscleral Drug Delivery: This involves delivering drugs through the sclera, bypassing the cornea and conjunctiva. It can be achieved by various methods, including iontophoresis, ultrasound, and microneedles.
- Suprachoroidal Injection: Therapeutics are injected directly into the choroid using ultrasound guidance reducing any risk of damaging the retina. Suprachoroidal delivery has the potential to prolong drug retention and maintain therapeutic drug levels in the eye over an extended period. Suprachoroidal delivery can reduce the frequency of dosing intervals, reducing the treatment burden for patients and improving treatment adherence.

Medical Testing
- Pachymetry: Ultrasound imaging is used to calculate the thickness of the cornea throughout perfusion. This is used as a marker of eye health indicating levels of oedema or dehydration within the eye. This non-invasive technique can be used to monitor metabolic activity within the cornea over the course of a perfusion.
- Intraocular Pressure Measurement: Use a tonometer to measure intraocular pressure, as elevated pressure can be a sign of glaucoma. Alternatively, Pebble can ulitise a direct measurement from within the eye using a pressure transducer to continuously monitor IOP. These measurements can be taken from either the antirior chamber or the vitreous cavity.
- Efficiency of Drainage Mechanisms: Study the dynamics of fluid flow within the eye without interference from other physiological factors. By monitoring changes in IOP, Pebble can assess the efficiency of the eye’s drainage mechanisms, such as the trabecular meshwork. Abnormalities in these structures can lead to increased resistance to aqueous humor outflow and elevated IOP, which is a major risk factor for glaucoma.
- Impact of Pharmacological Agents: Drugs that enhance aqueous humor outflow or reduce its production may lower IOP, while substances that disrupt drainage pathways may elevate IOP. Understanding how different compounds affect IOP can inform the development of new treatments for ocular conditions such as glaucoma.
- Pressure-Volume Curves: Understanding the pressure-volume characteristics of the eye is crucial for optimising surgical techniques and assessing the efficacy of implantable devices used in ophthalmic procedures. By analyzing pressure-volume curves, Pebble can evaluate the impact of surgical interventions, such as trabeculectomy or glaucoma drainage device implantation, on ocular biomechanics and intraocular pressure dynamics. This knowledge informs surgical decision-making, enhances treatment outcomes, and minimizes the risk of complications associated with ocular surgery.
- Evaluation of Pharmacological Agents: Administer pharmacological agents directly to the ocular tissue and study their effects on retinal function. By combining ERG recordings with perfusion experiments, Pebble can assess how drugs influence various aspects of retinal physiology, such as photoreceptor sensitivity, synaptic transmission, or ion channel activity. This information is crucial for identifying potential therapeutic compounds and optimizing treatment strategies for retinal disorders.
- Validation of Drug Delivery Strategies: Tear film analysis is essential for evaluating the efficacy of drug delivery strategies designed to enhance ocular bioavailability and therapeutic outcomes. By measuring tear film composition, drug concentration, and residence time, Pebble can assess the efficiency of drug delivery systems, such as eye drops, ointments, or contact lens-based drug delivery devices. Incorporating tear film analysis into ex vivo perfusion studies allows researchers to optimise drug formulations, delivery techniques, and treatment regimens to maximise therapeutic efficacy while minimising side effects and ocular surface toxicity.
- Assessment of Tear Film Dynamics: Study tear film dynamics in a controlled environment, free from confounding factors such as blinking or tear evaporation. By analysing tear film thickness, lipid layer characteristics, and mucin distribution, researchers can elucidate the mechanisms underlying tear film stability and tear film interactions with the ocular surface. Understanding tear film dynamics during ex vivo perfusion helps researchers identify factors contributing to tear film instability, ocular surface inflammation, or epithelial damage, which are common features of ocular surface disorders.
- Detection of Metabolic Imbalances: Assess the metabolic status of ocular tissues by measuring parameters such as pH, partial pressure of carbon dioxide (PCO2), and bicarbonate (HCO3–) levels. Deviations from normal values may indicate metabolic acidosis or alkalosis, which can adversely affect cellular metabolism, ion transport, and enzyme activity. By monitoring venous blood gases, Pebble can identify metabolic imbalances and adjust perfusion parameters or experimental conditions to maintain physiological pH and acid-base homeostasis in ocular tissues.
- Assessment of Corneal Health: Endothelial cells play a vital role in maintaining corneal transparency and hydration by regulating fluid balance within the cornea. Monitoring endothelial cell count during ex vivo perfusion provides valuable information about the health and functional capacity of the corneal endothelium. Changes in endothelial cell density can indicate endothelial cell loss due to aging, disease, surgical trauma, or other insults. A decrease in endothelial cell count may compromise corneal integrity, leading to corneal edema, decreased visual acuity, and increased susceptibility to corneal pathology.
Validation of Drug Effects: Ex vivo porcine eye perfusion can be used to evaluate the pharmacokinetics and pharmacodynamics of ocular medications. Endothelial cell count serves as a sensitive biomarker for assessing the cytotoxicity, tissue compatibility, and ocular safety of drug formulations. Changes in endothelial cell density following drug exposure can indicate potential adverse effects on corneal endothelial health, such as cell death, morphological alterations, or functional impairment. Monitoring endothelial cell count allows researchers to identify drugs with favorable ocular safety profiles and optimize drug formulations to minimize cytotoxicity and maximize therapeutic efficacy.
Quality Control & Standardisation: Endothelial cell count serves as a quality control measure for ex vivo porcine eye perfusion experiments. Establishing baseline endothelial cell density values for donor eyes ensures consistency and reproducibility across experimental studies. Deviations from normal endothelial cell counts may indicate variations in tissue quality, donor age, storage conditions, or experimental procedures that could influence study outcomes. By standardizing endothelial cell counting techniques and criteria, Pebble enhances the reliability and validity of ex vivo perfusion experiments and facilitate comparisons between different studies.
- Assessment of Ocular Surface Integrity: Ocular surface staining techniques can reveal areas of epithelial damage, defects, or irregularities that may result from experimental manipulations, surgical procedures, or pathological conditions. By assessing the extent and severity of ocular surface staining, Pebble can identify areas of compromised epithelial barrier function and investigate the underlying mechanisms of tissue injury or dysfunction.
- Detection of Dry Eye Phenotypes: Ex vivo porcine eye perfusion models are often used to study ocular surface diseases, such as dry eye syndrome, that affect tear film dynamics, epithelial integrity, and ocular surface health. Ocular surface staining provides a sensitive and quantitative measure of dry eye severity and phenotype by highlighting areas of epithelial disruption, punctate epithelial erosions, or corneal staining patterns indicative of tear film instability or inflammation. By correlating staining findings with clinical signs and symptoms of dry eye, researchers can characterize disease phenotypes, elucidate underlying pathophysiological mechanisms, and develop targeted therapeutic interventions.
- Evaluation of Therapeutic Interventions: Ocular surface staining serves as a valuable tool for assessing the efficacy of therapeutic interventions aimed at improving ocular surface health and treating ocular surface diseases. By performing staining assays before and after treatment administration, Pebble can quantitatively evaluate changes in staining patterns, epithelial integrity, and tear film stability. Reductions in ocular surface staining following treatment may indicate improvements in epithelial barrier function, resolution of epithelial defects, or normalization of tear film dynamics. Staining techniques allow Pebble to objectively measure treatment outcomes, optimize therapeutic regimens, and identify novel therapeutic targets for ocular surface disorders.
Assessment of Vascular Function & Integrity: Haemodynamic parameters such as blood flow velocity, vascular resistance, and perfusion pressure provide valuable information about vascular function and integrity in the eye. Monitoring haemodynamics during ex vivo perfusion allows researchers to assess the patency of ocular blood vessels, the responsiveness of vascular smooth muscle cells to vasoactive stimuli, and the overall efficiency of blood flow regulation mechanisms. Changes in haemodynamic parameters may indicate vascular dysfunction, endothelial damage, or alterations in tissue perfusion that contribute to ocular pathology.
Evaluation of Pharmacological Interventions: Haemodynamic measurements can be used to assess the effects of pharmacological agents on ocular blood flow, vascular tone, and tissue perfusion. By monitoring haemodynamics during drug administration, researchers can evaluate drug efficacy, bioavailability, and safety profiles, as well as identify potential side effects or adverse reactions related to alterations in ocular haemodynamics. Understanding how drugs influence ocular haemodynamics is essential for optimizing treatment strategies and developing novel therapeutic interventions for ocular diseases.
Validation of Surgical Techniques: Ex vivo eye perfusion models are valuable tools for evaluating the efficacy and safety of surgical procedures used to treat ocular diseases such as glaucoma, retinal vascular occlusions, and ocular trauma. Haemodynamic measurements can be used to assess the impact of surgical interventions on ocular blood flow, intraocular pressure, and tissue perfusion. By monitoring haemodynamics before, during, and after surgery, researchers can evaluate surgical outcomes, identify potential complications such as ischaemia or hypoperfusion, and optimize surgical techniques to minimise risks and improve patient outcomes.

Imaging
Assessment of Ocular Surface Integrity: Visualise the corneal and conjunctival surfaces in real time. By examining the ocular surface under magnification, Pebble can identify epithelial defects, abrasions, or irregularities that may occur during perfusion experiments. Staining techniques, such as fluorescein or lissamine green, can be used in conjunction with slit lamp examination to highlight areas of epithelial damage or compromise. Monitoring the ocular surface integrity during perfusion provides insights into the effects of experimental conditions, fluid dynamics, or pharmacological agents on corneal and conjunctival health.
Evaluation of Tear Film Dynamics: Assess tear film stability, distribution, and quality during ex vivo eye perfusion. By observing tear film breakup patterns, meniscus height, or debris accumulation, researchers can evaluate the dynamics of tear film production, distribution, and clearance. Changes in tear film characteristics may indicate alterations in tear film composition, ocular surface lubrication, or tear film stability induced by perfusion conditions or experimental interventions. Slit lamp examination provides a qualitative and quantitative assessment of tear film dynamics, facilitating the investigation of tear film physiology and pathology in ex vivo models.
Identification of Anterior Segment Abnormalities: Examine the anterior segment structures of the eye, including the cornea, anterior chamber, iris, and lens. By evaluating the clarity, transparency, and morphology of these structures, researchers can detect abnormalities such as corneal opacities, anterior chamber inflammation, iris abnormalities, or lens opacities. Slit lamp biomicroscopy allows for detailed visualization of anterior segment structures, enabling researchers to identify structural changes, pathological features, or adverse effects induced by perfusion conditions or experimental manipulations.
- Evaluation of Retinal Health: Fundus imaging allows for visualisation and assessment of the retina, including the optic nerve head, retinal vasculature, and peripheral retina. By capturing high-resolution images of the fundus, the Pebble Team can evaluate the structural integrity, morphology, and vascular perfusion of the retina during ex vivo perfusion. Changes in retinal appearance, such as optic disc edema, vascular leakage, or retinal hemorrhages, may indicate alterations in retinal health, perfusion dynamics, or tissue viability induced by perfusion conditions or experimental interventions.
- Monitoring of Retinal Blood Flow: Fundus imaging can be used to assess retinal blood flow dynamics and vascular function during ex vivo eye perfusion. Techniques such as fluorescein angiography or indocyanine green angiography allow for visualization of retinal circulation and assessment of blood flow patterns, capillary perfusion, and vascular leakage. Monitoring retinal blood flow parameters provides insights into ocular hemodynamics, vascular autoregulation, and the effects of perfusion conditions or pharmacological agents on retinal perfusion and tissue oxygenation.
- Assessment of Vascular Leakage: Detect and quantify vascular leakage or extravasation of fluorescein dye from retinal and choroidal blood vessels. Increased fluorescence intensity, dye pooling, or dye leakage into retinal tissue may indicate breakdown of the blood-retinal barrier, vascular permeability changes, or inflammatory processes induced by perfusion conditions or experimental manipulations. Monitoring vascular leakage using fluorescein angiography provides valuable information about retinal and choroidal vascular function, integrity, and response to therapeutic interventions in ex vivo models.
- Investigation of Pharmacological Effects: Evaluate the effects of pharmacological agents on retinal and choroidal vascular function, perfusion dynamics, and vascular leakage in ex vivo porcine eye perfusion experiments. By administering drugs or therapeutic compounds into the perfusion system and monitoring fluorescein angiography images, researchers can assess the impact of treatments on retinal and choroidal vascular parameters, such as vessel caliber, blood flow velocity, or vascular leakage rate. Fluorescein angiography provides quantitative and qualitative measures of drug efficacy, safety, and dose-response relationships, facilitating the development of novel treatments for retinal diseases and ocular conditions.
Evaluation of Retinal Pathology: OCT is particularly valuable for evaluating retinal pathology in ex vivo eye perfusion studies. It allows for visualisation and quantify various retinal abnormalities, such as retinal edema, intraretinal cysts, retinal detachment, or macular degeneration, with high sensitivity and specificity. By correlating OCT findings with histopathological analysis and other imaging modalities, Pebble can elucidate the structural and functional changes associated with retinal diseases and assess the efficacy of therapeutic interventions in ex vivo models.
Integration with Other Imaging Modalities: OCT can be integrated with other imaging modalities, such as fluorescein angiography (OCTA), fundus photography, or adaptive optics imaging, to provide comprehensive insights into ocular anatomy, function, and pathology. By combining multiple imaging techniques, researchers can obtain complementary information about tissue structure, perfusion dynamics, and cellular function, enhancing our understanding of ocular physiology and disease mechanisms in ex vivo eye perfusion studies.
- Hematoxylin and Eosin (H&E) Staining: H&E staining is one of the most widely used staining techniques in histology. Hematoxylin stains nuclei and other acidic structures blue-purple, while eosin stains cytoplasm and extracellular matrix components pink. H&E staining provides detailed information about tissue architecture, cellularity, and pathological changes, making it suitable for general histological examination of ocular tissues in ex vivo perfusion studies.
Periodic Acid-Schiff (PAS) Staining: PAS staining is used to detect carbohydrates and glycoproteins in tissues. It stains polysaccharides, glycogen, mucin, and basement membranes magenta. PAS staining is particularly useful for evaluating glycogen content in corneal endothelial cells, basement membrane thickness in retinal blood vessels, and mucin distribution on the ocular surface in ex vivo eye perfusion experiments.
Masson’s Trichrome Staining: Masson’s trichrome staining is used to distinguish between collagen, muscle, and other connective tissue components in tissues. Collagen fibers stain blue, muscle fibers stain red, and cell nuclei stain black. Masson’s trichrome staining is valuable for assessing fibrosis, scarring, and extracellular matrix remodeling in ocular tissues subjected to ex vivo perfusion conditions.
Van Gieson’s Staining: Van Gieson’s staining is a differential staining technique used to highlight collagen fibers and differentiate them from other tissue components. Collagen fibers stain red, while other tissue components stain yellow or brown. Van Gieson’s staining is useful for evaluating collagen content, distribution, and organization in ocular tissues, such as the sclera, cornea, and optic nerve, in ex vivo perfusion studies.
Alcian Blue Staining: Alcian blue staining is used to detect acidic mucopolysaccharides, such as glycosaminoglycans, in tissues. It stains mucin-rich structures, cartilage, and basement membranes blue. Alcian blue staining is commonly used to evaluate the distribution and composition of mucins in the tear film, conjunctiva, and corneal epithelium in ex vivo eye perfusion experiments.
Immunohistochemistry (IHC): Immunohistochemistry is a technique used to detect specific proteins or antigens in tissues using antibodies labeled with fluorescent or chromogenic markers. IHC allows researchers to localize and quantify the expression of specific proteins or biomarkers associated with cellular function, differentiation, or disease processes in ocular tissues subjected to ex vivo perfusion conditions.

Cell Analysis
- Whole Genome Sequencing (WGS): This technique involves sequencing the entire DNA content of an organism. WGS can be used to identify genetic variations associated with eye diseases or conditions.
- Genome-Wide Association Studies (GWAS): GWAS analyse variations in the DNA sequence to identify genetic factors associated with specific eye disorders.
- RNA Sequencing (RNA-Seq): This method quantifies and analyses the entire transcriptome of a cell or tissue, providing information about gene expression levels. It can be used to study changes in gene expression in different parts of the eye or under various conditions.
- Mass Spectrometry: Mass spectrometry can be employed to identify and quantify proteins in the eye. This helps in understanding the proteomic profile of different eye tissues and detecting changes associated with diseases.
- 2D Gel Electrophoresis: This technique separates proteins based on charge and molecular weight, enabling the comparison of protein profiles in healthy and diseased eyes.
- Nuclear Magnetic Resonance (NMR) Spectroscopy & Mass Spectrometry: Metabolomics analyses the small-molecule metabolites in a biological sample. It can provide insights into the metabolic pathways and changes associated with eye diseases.
- DNA Methylation Analysis: DNA methylation patterns can be studied to understand epigenetic regulation in the eye. Changes in DNA methylation may be associated with various eye disorders.
- Histone Modification Analysis: Studying modifications to histone proteins can reveal information about the chromatin structure and gene regulation in ocular tissues.
- Mass Spectrometry & Chromatography: Glycomics focuses on the study of the structure and function of carbohydrates (glycans). Analysing the glycome of the eye can provide insights into the roles of glycoproteins and glycolipids in eye health and disease.
- Mass Spectrometry: Lipidomics involves the identification and quantification of lipids. Studying the lipid profile of the eye can help understand the role of lipids in maintaining ocular structure and function.
Pebble's Customisable Service Package